The views expressed in our content reflect individual perspectives and do not represent the authoritative views of the Baha'i Faith.
Baha’u’llah, the prophet and founder of the Baha’i Faith, spent the last forty years of his life in exile and prison. The teachings of his new Faith—world unity, the common foundation of all religions, the equality of men and women, global peace and harmony—so angered the Islamic clerical authorities that they persecuted Baha’u’llah mercilessly, finally sentencing him and his family and followers to a notoriously malarial prison colony in Akka, Palestine:
We had no communication whatever with the out-side world. Each loaf of bread was cut open by the guard to see that it contained no message. All who believed in the Baha’i manifestation, children, men and women, were imprisoned with us. There were one-hundred and fifty of us together in two rooms and no one was allowed to leave the place with the exceptions of four persons, who went to the bazaar to market each morning, under guard. The first summer was dreadful. Akka is a fever-ridden town. It was said that a bird attempting to fly over it would drop dead. The food was poor and insufficient, the water was drawn from a fever-infected well and the climate and conditions were such, that even the natives of the town fell ill. Many soldiers succumbed and eight out of ten of our guard died. During the intense heat, malaria, typhoid and dysentery attacked the prisoners, so that all, men, women and children, were sick at one time. There were no doctors, no medicines, no proper food, and no treatment of any kind. – Abdu’l-Baha, Abdu’l-Baha in London, pp. 115.
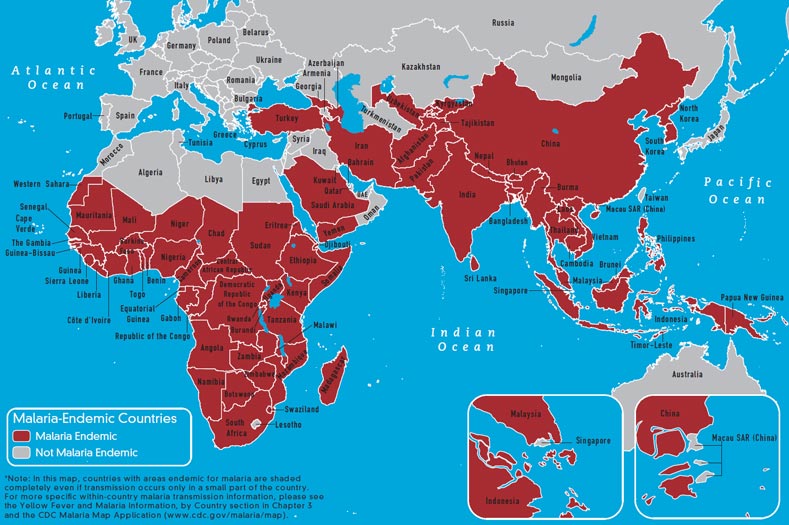
Residents of that region of Palestine (now Israel) probably received infectious bites from Anopheles mosquitoes in cities and towns, because one species called Anopheles claviger had adapted to the underground cisterns used to hold fresh water. Another mosquito species and malaria carrier, Anopheles sacharovi, lived in the grassy, freshwater marshes of the rural plain between Akka and Haifa.
People have long suffered from malaria, historically associated with the emergence of human civilization. Sanskrit, Greek, and Chinese medical texts all gave detailed descriptions of the episodic fevers from malaria. The ancient Chinese called malaria “chang chi” which translates roughly to “malicious air,” precisely the meaning in the Italian from which the word “mal” (bad) “aria” (air) comes from.
These names relate to the idea that in swampy, wet areas one would breathe the bad air or miasma emanating from the environment, and the symptoms of malaria (acute cycles of chills and fevers in particular) would ensue. For thousands of years, though, no one knew the true cause of malaria. However, coincident with the explosion of scientific knowledge of the late 19th century, the French-Algerian physician Alphonse Laveran, working in North Africa in 1878, discovered the malaria parasite in the blood of an ill soldier. Later, the British colonial physician Ronald Ross in India in 1898 conducted experiments with bird malaria that proved parasite transmission by mosquitoes. The Italian entomologist Giovanni Battista Grassi did similar experiments with Anopheles mosquitoes and humans at the same time near Rome. These findings revolutionized the medical field; both Ross and Laveran were ultimately awarded the Nobel Prize for Medicine for their accomplishments—although poor Grassi unjustly didn’t share the prize.
Because scientists recognized malaria as not only a serious illness for individuals, but also a restraint on social development and intertwined with poverty, movements began to form, sometimes with colonial or military motivations but in other cases for humanitarian reasons, to control and eradicate the disease. These movements began shortly after Ross and Grassi made their discoveries and published them. Many regions successfully eradicated malaria, but it remains an extremely important problem in tropical areas and particularly in the so-called Lesser Developed Countries.
A world wide attempt to eradicate malaria began after World War II, under the auspices of the newly-organized World Health Organization. Based on the use of indoor sprays of long lasting insecticides such as DDT and new drugs such as chloroquine, which both emerged from scientific investigations demanded by the war effort, it worked effectively in many regions–but by the late 1960s many national programs had reversed and malaria resurged to pre-eradication levels.
A recent analysis by Dr. Justin Cohen of the Clinton Foundation indicates that insecticide and drug resistance did not cause these failures–but rather the inability to sustain the programs in the face of costs and the unchanged social context of poverty. Throughout this era, a divergence of thought occurred. One group, those who relied on material means, had faith in the new technical prowess provided by the chemical industry, and promoted certain post-colonial models of economic development. The other group, the less-heard but poignant voices of those who emphasized the humanitarian basis for malaria control, focused on the need to address the root of the problem: poverty.
A great debate still rages over whether malaria makes poverty, or poverty makes malaria.
All the research shows strong relationships between the two. My own research collaboration in southern Malawi demonstrated that marginal increases in the household wealth of poor people are associated with marked declines in risk of malaria. Fascinating research in western Kenya by Dr. Kacey Ernst of the University of Arizona showed that when women in poor, rural households have marginally higher levels of formal education, the risk of malaria for everyone in those households declines substantially. The questions now arising have to do with whether malaria can properly be controlled technically and with the right weapons; or if malaria needs to be viewed as a problem of social justice. The answer: undoubtedly both, with the latter required to balance the former.
Control of malaria, leading to elimination of it globally, became a renewed focus of international effort in 2000 with the Millennium Summit, with tremendous support from the public, private, and philanthropic sectors. New international networks and funding mechanisms emerged; and in one sense malaria itself became a unifying force, leading to some notable successes.
Malaria deaths globally have dropped by a third and the malaria distribution map has shrunk. Child survival is up. Women have become a primary focus, with distribution of insecticide treated bed nets by the millions through rural, antenatal clinics; and the provision of intermittent, preventive drug therapies to pregnant women, a particularly high-risk group. The current and recognizably ambitious Millennium goal aims to reverse malaria incidence (recruitment of new cases) from a positive to a negative number by 2015.
We still have a long way to go before we eliminate malaria, and many obstacles to overcome. But the collective decision-making involved, the global consciousness of the problem, and the concerted action across a wide spectrum of society all represent a great sign of our time, a true world undertaking that fulfills Abdu’l-Baha’s promise.








Comments
Sign in or create an account
Continue with Googleor